As agencies across the country have been grappling with a new wave of customers seeking help due to the COVID-19 health crisis, they must now prepare for the massive number of existing customers who must be renewed after the public health emergency (PHE) and pandemic waivers come to an end.
With Medicaid enrollment up 18 percent since February 2020, representing more than 12 million additional individuals nationally, and Supplemental Nutrition Assistance Program (SNAP) enrollment up nearly 15 percent, agencies are simultaneously managing unprecedented enrollment, facing the capacity challenges associated with the end of PHE, and ensuring their service delivery systems align with federal guidelines for conducting renewals, even as those guidelines continue to shift. Medicaid enrollment has grown to nearly 84 million individuals nationally, all of whom will need to be reviewed after the end of the PHE. All of this is occurring at a time when labor shortages are making it increasingly difficult to retain and hire staff.
The daunting task of re-engaging customers to ensure those who meet eligibility guidelines continue to maintain services—many of whom may have not updated their contact information for more than two years—will significantly impact and hamper agencies as they work to help families in need. Customers will potentially lose important benefits and agencies’ workload will increase. This workload growth will be larger than the number of customers requiring renewal services. In many states today, for every one customer contacting the agency to access services, four customers are navigating the process — pursuing answers to questions such as “What is the status of my case? May I reschedule an appointment? I submitted my verification, so when will I get my benefits?” Churn will also be a factor. When customers realize they have lost benefits, agencies will face even more work by responding to calls about the status of benefits, resending requests for information, and processing new applications for customers who could have remained eligible in the first place.
Is it any wonder that human services agencies feel as if they are being tasked with building a plane while it is already in the air? Without a solid plan to increase capacity, this unique set of circumstances will lead to a capacity crisis in all work areas; there simply won’t be sufficient staff bandwidth to handle the increased demand. The influx of customer visits and calls will overwhelm even the best operated service delivery systems in the country.
The Impact of Self-Created Workload
Recovering organizational capacity to meet this increased demand requires that agencies clearly understand the practices in service delivery that erode valuable staff time.
Our work in 25 state agencies illustrates the general customer experience that occurs in a capacity-drained agency: a family initiates a request and around 15 to 20 days later the agency decides to either approve and continue services or deny the request. Certainly, some customers get a decision sooner, but others will wait for a decision for perhaps 30 or 45 days.
Another common observation that we see in many states is that, on average, from the time the customer submits an initial request until a decision is made, agencies spend about two hours of staff time, collectively, on a single case. What in the process turned two hours of work into a 20-day wait for our customers? This is such an important question because the longer work remains “unfinished” in our systems, the greater the likelihood of the customer interacting with the agency multiple times as they seek to understand the status.

Diagram 1
Reality Check
To get a good indication of the potential opportunity to eliminate self-created workload in your agency, compare the number of applications and renewals in any given month against the volume of calls and office visits your agency receives. Usually, it’s not even close. For every single customer contacting you to initiate a service, four more customers are navigating the process, asking for a status update, rescheduling an appointment, or calling to make sure verification was received.
These repeat and often unnecessary interactions with the same customers are what erodes staff capacity. What we discovered from our work with these states is that the average customer interacted with the state or county agency, in person or virtually, three to five times in the course of a single eligibility event.
UK management guru John Seddon calls this “failure demand.” It is the extra work we create when we do not provide decisions at first interaction—whether it is in person, online, or over the phone. Even worse from a capacity standpoint, this self-created workload does not just mean repeat interactions, it causes work that must be managed and tracked. When agencies are dealing with a high volume of unfinished work, they create new processes to manage that work, dedicating valuable staff time to manage these processes and respond to unnecessary customer interactions. Eventually states invest incredible resources for IT solutions to enable their ability to track and provide the status of the unfinished work.
Focusing on On-Demand Services and First Contact Resolution
When agencies do not have a robust, on-demand, same-day service and First Contact Resolution strategy, the impact on agencies is significant. Here is an example (see diagram 2): We recently worked with one of the largest state-administered agencies in the country; they process 290,000 applications and renewals each month. Initial processing of each application or renewal resulted in a request of additional information rather than a decision for 6 out of every 10 customers. When we measured the number of visits and calls, at least those we could quantify, the state recorded 1.2 million customer interactions every month. In addition to the staff working in field offices and processing centers, this state also dedicated millions of dollars annually for a vendor to staff a call center that only provided customers with answers about the status of cases. This back and forth created additional unnecessary handoffs to already overburdened state staff, adding processing delays, and forcing even more customer calls and visits. While well intentioned, these approaches did not deliver the desired outcome because they did not address the underlying problem. The agency would have had a better outcome by focusing on creating an avenue for resolving customer needs with state staff, or better yet, eliminating the reasons that led to customers’ calls.
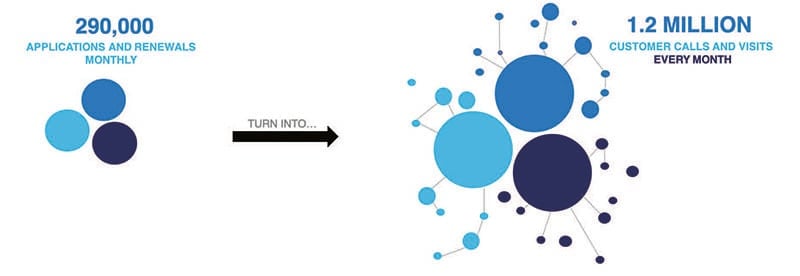
Diagram 2
Strategies to Regain Capacity
Self-inflicted work created the challenges outlined above. Unwinding process and policy changes implemented during the PHE will compound those challenges. Without taking strategic action to prepare for PHE unwinding, human services agencies are at risk of overwhelming their systems and staff, leading to backlogs of work. Not only do backlogs mean that eligible individuals wait longer for services, but they also contribute to agencies continuing to pay for services for ineligible individuals whose cases have not yet been reviewed.
Strategy 1: Make the work visible
Planning for needed capacity begins with understanding the inevitable influx of work and ensuring that the workload is visible. States must use current and historical data to understand the volume of work that will be received once normal operations are resumed and the types of work that will be represented. For example, based on guidance issued by the Centers for Medicare and Medicaid Services (CMS) in August 2021, Medicaid agencies will be expected to complete pending eligibility and enrollment actions within 12 months after the month in which the PHE ends. This guidance also requires agencies to complete a redetermination after the end of the PHE before terminating coverage for an individual. Considering Medicaid enrollment growth of 20 percent during the pandemic, these requirements mean that states will have to complete 20 percent more renewals in the year following the PHE than they were accustomed to completing prior to the pandemic. This work will be combined with normal applications and changes, and agencies should use their existing data sources and historical information to project workloads based on enrollment, historic auto-renewal and return rates, historic volume of applications and changes, and any historical data about application churn resulting from closures. Due to staff attrition during the PHE and expected upcoming workload, one Medicaid agency projects a need to hire 50 percent more eligibility workers to accommodate the workload.
This focus on data and visibility will be crucial for managing the workload and is included in CMS’ recommendations that states have adequate tracking and management tools to monitor case volume, renewal rates, and workforce needs.
Today’s eligibility systems and promises of no-touch decisions are yielding inadequate results for states. Worse yet, states receive an inordinate number of data “matches,” most of them recommended and sometimes mandated in some fashion, pertaining to active or pending cases.
Strategy 2: Make the work flow better
Predicting and tracking incoming work is not enough. That work must also be prioritized and delivered to workers in a way that ensures as many customers as possible are served with the available resources each day. Whether in line, online, or via call center, processes should be designed to put our expertise up front and serve the customer completely the first time, every time. Connecting customers with the next available worker skilled to resolve their specific needs increases the likelihood of resolving customers’ issues at first contact and moves agencies toward more timely eligibility decisions.
Strategy 3: Make the work smarter: Leverage validated, current, and better data to do the work for you
There is tremendous opportunity with determining and monitoring eligibility in real time without workers having to manually search for verifications, relying on old and incomplete data, or worse yet, waiting days for customers to return information. Using authoritative, real-time, and better quality data available via commercial and public sources helps agencies reduce workload. While the data are part of the value, the real value is what states can do with it: provide curated results customized to their program rules to enable real-time insights and verification. This allows agencies to validate customer circumstances in real time, increase staff capacity, and reduce customer churn, thus avoiding an unnecessary break in coverage for eligible customers.
Today’s eligibility systems and promises of no-touch decisions are yielding inadequate results for states. Worse yet, states receive an inordinate number of data “matches,” most of them recommended and sometimes mandated in some fashion, pertaining to active or pending cases. These data would be helpful if they were indeed relevant, material, and actionable. However, the vast majority of data matches such as the National Directory of New Hires, the Public Assistance Reporting Information System, and Departments of Corrections, to name a few, are simply noise because the information is old, unreliable, or provides false positives, requiring staff to sift through the matches in order to meet requirements or find something with material value to a case.
Every one of these work tasks resulting from a data match requires a manual process to search for what data are useful and actionable. Staff review them one by one to determine what, if anything, needs action. Most do not require action based on the issues articulated above—they are largely irrelevant for one reason or another.
Using real-time and validated data sources, customized to states’ rules, decreases administrative burden by minimizing the number of customer interactions required. For Medicaid states conducting auto-renewals, real-time and validated data sources yield higher no-touch rates without any need for worker or customer involvement. And for those customers experiencing material changes, pre-filling renewal forms with known, real-time, authoritative information for customers to validate, sign, and return further reduces churn and self-created work for agencies.
Decreasing the administrative burden to obtain or keep coverage provides immediate benefits to both customers and agencies. Ensuring that eligible individuals retain coverage avoids gaps in health care for individuals and decreases application churn from individuals who lose coverage and then reapply. Decreased administrative burden also leads to faster processing. For Medicaid agencies that have been subjected to a continuous enrollment requirement during the PHE, time is money. The faster they process renewals within the boundaries of CMS’ guidelines, the more ineligible payments will be reduced. Ultimately, agencies have a shared goal to ensure that eligible customers receive their benefits. At renewal, agencies have an opportunity to do so by improving no-touch auto-renewals, pre-filling renewal forms, and seamlessly transferring Medicaid-ineligible individuals to health care exchanges.
As PHE waivers end and your agency’s workload increases, these strategies will help your agency face the future and navigate the influx of demand that is on its way. With your leadership and agency’s will, drive, and never-ending commitment to transform its service delivery, you can apply these practices quickly.
The best way to meet the crushing workload of PHE is to serve customers completely, immediately. This requires visibility into the pile of work, technology, and practices to route the right work to the right worker at the right time and the use of data and insights to provide real-time verification, validation, and pre-population. Done right, the PHE solution can be as easy as pushing a button.
[fusion_separator style_type=”single solid” hide_on_mobile=”small-visibility,medium-visibility,large-visibility” class=”” id=”” sep_color=”#606060″ top_margin=”25px” bottom_margin=”1px” border_size=”” icon=”” icon_circle=”” icon_circle_color=”” width=”45%” alignment=”left” /][fusion_text]
*Originally published as Emerging Stronger When the Public Health Emergency Ends: How Agencies Can Make Room for the Upcoming Wave of Renewals and New Customers (Policy & Practice, February 2022)







